A Comprehensive Guide to Pancreatitis: Types, Symptoms, Diagnosis, and Treatment

Pancreatitis refers to the condition when your pancreas gets inflamed, swollen, and irritated. It is not a typical medical issue. Multiple factors contribute, but gallstones and excessive alcohol consumption are often at fault. The condition might manifest itself quickly or persist over time. Either way, it poses severe health risks.
Here is an extensive guide on pancreatitis that covers all aspects of the condition, from causes and symptoms to treatment and prevention.
What Is Pancreatitis?
When digestive enzymes start acting before your pancreas secretes them, the pancreas could be harmed, causing tissue damage and inflammation of the organ. The kidneys, lungs, and heart can all be negatively impacted by an inflamed and irritated pancreas, which can also produce inflammatory cells and toxins.
There are two types of pancreatitis:
Acute Pancreatitis
Acute pancreatitis is characterized by rapid onset and rapid resolution. The symptoms can be quite modest or may progress to a point where they threaten one's life. In its most severe forms, acute pancreatitis can result in hemorrhaging, serious tissue damage, infections, and cysts. Severe pancreatitis can harm your heart, lungs, kidneys, and pancreas, in addition to other organs.
The vast majority of people with acute pancreatitis recover completely after receiving proper care.
Chronic Pancreatitis
It's a prolonged and persistent inflammation of the pancreas. Commonly, it occurs following a bout of acute pancreatitis. Heavy, chronic alcohol consumption is another major contributor.
Drinking excessively can harm your pancreas permanently, which may go undetected for years before developing into chronic pancreatitis.
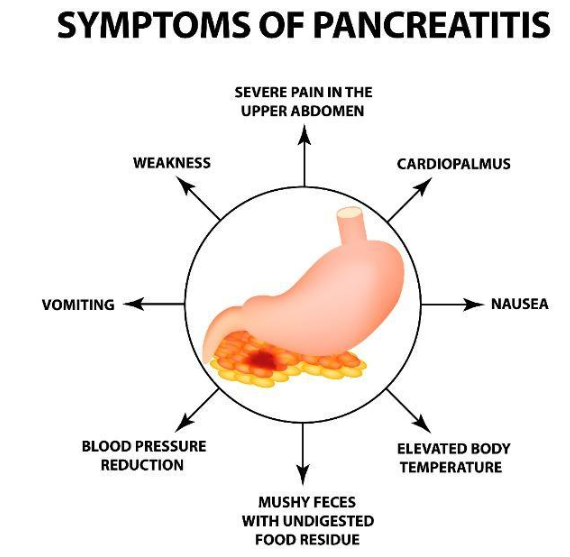
Most Common Symptoms of Pancreatitis
The signs and symptoms of pancreatitis differ from person to person, depending on the type of pancreatitis you experience.
Signs and symptoms of Acute Pancreatitis include:
- Pain in your upper abdomen
- Backache that originates in the abdomen
- Fever
- Nausea
- Pain or discomfort felt when pressing the abdomen
- Increased heart rate
- Vomiting
Signs and symptoms of Chronic Pancreatitis include:
- Pain in your upper stomach
- Stomach ache that worsens after eating
- Unintended weight loss
- Steatorrhea
Key Causes and Risk Factors Associated with Pancreatitis
Some of the most common reasons why people get Acute Pancreatitis are:
- Immune-mediated disease
- Gallstones
- Consuming large amounts of alcoholic beverages
- Infections
- Surgical procedure
- Conditions involving the metabolism
- Trauma
The following can lead to Chronic Pancreatitis:
- Gallstones
- Medications
- A high level of triglycerides
- Regular alcohol consumption
Pancreatitis risk factors consist of the following:
Drinking Too Much
Evidence suggests that heavy drinkers who consume four or more drinks per day are more likely to develop pancreatitis.
Obesity
Pancreatitis is more prevalent in the obese.
Diabetes
Developing pancreatitis is more likely in those with diabetes.
Smoking Cigarettes
Chronic pancreatitis occurs among smokers at a rate multi folds faster than among nonsmokers.
Family History of Pancreatic Disorders
More and more evidence point to a hereditary element in chronic pancreatitis. Your chances are higher if you have a family history of the disease, and they rise even further when you include additional risk factors.
Diagnosis of Pancreatitis
The presence of symptoms or risk factors, such as persistent excessive alcohol consumption or gallstone disorders, may lead your doctor to diagnose pancreatitis. You may need to undergo more testing to get a definitive diagnosis.
Diagnosis for Acute Pancreatitis
Blood tests measuring pancreatic enzyme levels of amylase and lipase are commonly ordered to diagnose acute pancreatitis. Excessive concentrations of these enzymes characterize these conditions. Inconsistencies in your pancreas, gallbladder, or bile duct can be seen on an ultrasound or CT scan by a doctor.
Diagnosis for Chronic Pancreatitis
Chronic pancreatitis requires a more thorough evaluation to diagnose. The doctor may recommend the following tests:
Oral glucose tolerance test
If your doctor feels that pancreatitis has destroyed the cells located in your pancreas that produce insulin, he may order this test. A blood sample is taken before and an hour after ingesting a sugary drink to see how well your body processes the sugar.
Secretin pancreatic function test
The responsiveness of your pancreas to secretin, a hormone produced in your small intestine, is measured here. The pancreatic secretion that digests juice is normally triggered by secretin. A medical expert will inject secretin and then measure the response by passing a tube down the patient's throat, past the stomach, and into the uppermost part of the small intestine.
Endoscopic ultrasound (Endosonography)
Your pancreas and its ducts can be seen more clearly on an
internal endoscopic ultrasound. A healthcare provider will place a small ultrasound instrument on the end of a thin tube and insert it down your throat, into your stomach, and then into your small intestine.
Your pancreas, a section of your liver, your gallbladder, and your bile duct will all be imaged in great detail by the endoscopic ultrasound.
Stool test
If you have digestive issues and your doctor suspects that you are having trouble metabolizing fat, they may perform a stool test.
ERCP (Endoscopic Retrograde Cholangiopancreatography)
A tiny camera is inserted into a tube down the patient's neck, through the stomach, and into the small intestine down to the ampulla, which is where the bile duct and pancreatic duct meet.
Then, the bile duct and pancreatic duct get injected with dye. Your doctor will be able to see your pancreas and bile duct clearly with this test. A gallstone, pancreatic stone, or anything else obstructing the bile duct can be surgically removed.
Treatment of Pancreatitis
Treatment for Acute Pancreatitis
Acute pancreatitis can cause severe discomfort. Therefore, doctors may prescribe powerful painkillers. Having a tube inserted into your nose and into your stomach to drain its contents may be necessary. If the procedure lasts a bit longer, you may also be given fluids and nutrients intravenously.
A hospital stay is likely, and you may receive the following treatment there:
- A dose of antibiotics if your pancreas gets infected.
- Intravenous (IV) fluids get administered via a needle.
- Recommended intermittent fasting or a low-fat diet. Fasting will likely help your pancreas heal. A feeding tube could be utilized to provide nourishment in this scenario.
- Medications to relieve discomfort.
More severe cases may require treatments that include:
- Endoscopic retrograde cholangiopancreatography (ERCP).
- Gallbladder surgery, in the case of pancreatitis, was caused by gallstones.
- Fluid or diseased tissue removal from the pancreas through surgery.
Treatment for Chronic Pancreatitis
If you suffer from Chronic Pancreatitis, your doctor will prioritize relieving your pain while minimizing the risk of you becoming addicted to medicines prescribed to you and keeping an eye out for problems that may damage your digestive system.
Most likely, the medical experts would prescribe
pancreatic enzyme replacement therapy to reestablish the digestive tract's capability to absorb foods and nutrients. It will probably also lower the number of times you experience new attacks.
You would require:
- Pain medications.
- Insulin is used in the treatment of diabetes.
- Pancreatic enzymes assist your body in absorbing an adequate supply of nutrients from the food consumed.
- Surgical operations or other procedures to alleviate discomfort, assist with drainage, or treat obstructions.
- An injection of anesthetics into the nerves close to your spine to help relieve the pain. If the pain is not alleviated by medicine or nerve blocks, the compromised pancreatic tissue might be surgically removed as a final option.
Treating Pancreatitis at Home
After being discharged from the hospital, you can continue your rehabilitation from pancreatitis by taking measures such as:
- Stopping alcohol consumption is recommended when healing from pancreatitis, regardless of whether or not alcohol consumption was a contributing factor. Seek medical advice if you can't quit drinking by yourself.
- Put an end to your smoking habit. Don't take up smoking if you don't already. Get medical assistance if you find that you cannot quit smoking on your own. Nicotine withdrawal is difficult, but medication and therapy can help.
- Eat more vegetables and fruits, healthy grains, and lean proteins, and cut back on the amount of fat you eat.
- Increase your fluid intake. As pancreatitis can lead to dehydration, it's essential to maintain a steady fluid intake all day.
How Can You Prevent Pancreatitis?
We should always remember that prevention is always better than cure. Pancreatitis can generally be prevented by cutting back on or giving up alcohol, as this is the underlying cause of several cases.
Consult your physician or a medical expert about alcohol treatment options if your alcoholism is causing you or others concern. It may also be helpful to join a support group.
Finally, to experience reduced and milder incidents of pancreatitis, you should give up smoking, exercise regularly, follow the diet recommendations from your doctor and dietician, and pursue your medication routine as prescribed.
When it comes to gastroenterology-related conditions,
Northlake Gastroenterology Associates is your best bet for cutting-edge diagnostics and care in Southeast Louisiana. Our highly experienced medical staff is qualified to treat various upper and lower gastrointestinal tract conditions, such as pancreatitis, Barrett's esophagus, ulcerative colitis, Crohn's disease, indigestion, constipation, and several other complications.
If you have any questions or concerns, please don't hesitate to get in touch with us or
book an appointment. We are here for you whenever you have any of these issues so that we can help you resolve them and get you back on track to a happy, healthy life.
More Blogs